2025-06-17 バース大学
<関連情報>
- https://www.bath.ac.uk/announcements/prescribing-fewer-antibiotics-might-not-be-enough-to-combat-threat-of-superbugs-says-new-research/
- https://www.sciencedirect.com/science/article/pii/S2213716525001092
ワンヘルスを運用するための橋渡し – 臨床および廃水ベースのサーベイランスアプローチを用いたイングランドにおける2年間の縦断的AMR研究 Building bridges to operationalize One Health — A longitudinal two years’ AMR study in England using clinical and wastewater-based surveillance approaches
Like Xu, Nicola Ceolotto, Kishore Jagadeesan, Richard Standerwick, Megan Robertson, Ruth Barden, Helen Lambert, Barbara Kasprzyk-Hordern
Journal of Global Antimicrobial Resistance Available online: 12 May 2025
DOI:https://doi.org/10.1016/j.jgar.2025.05.005

HIGHLIGHTS
- Reductions in antibiotic (AB) consumption and AMR prevalence during the COVID pandemic were observed.
- Reductions in AB and AMR were most significant during lockdowns.
- Reduction in AB/AMR is likely due to limited social interactions rather than reduced AB prescribing.
- Implications for policy that focuses on reduced AB prescription as an AMR management strategy.
- More holistic One Health strategies are needed to address the AMR challenge.
ABSTRACT
Objectives
The coronavirus disease 2019 (COVID-19) pandemic impacted antimicrobial resistance (AMR) in clinical settings, but evidence is lacking. Considering this, we evaluated community-wide AMR in the shadow of COVID-19, using wastewater-based epidemiology (WBE).
Methods
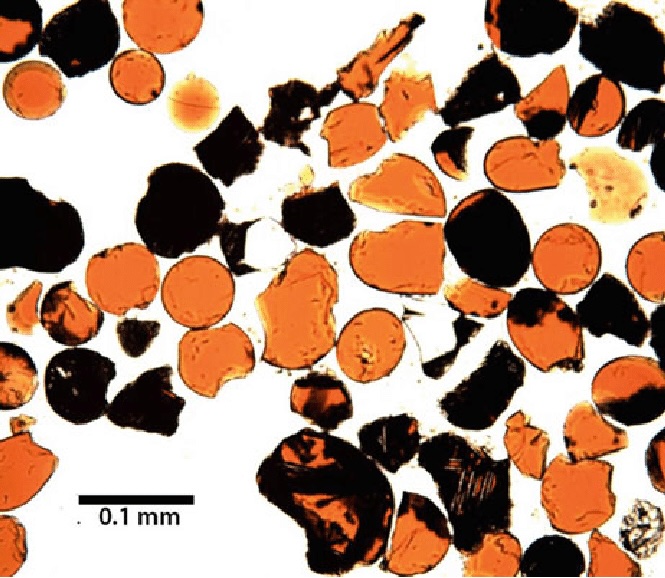
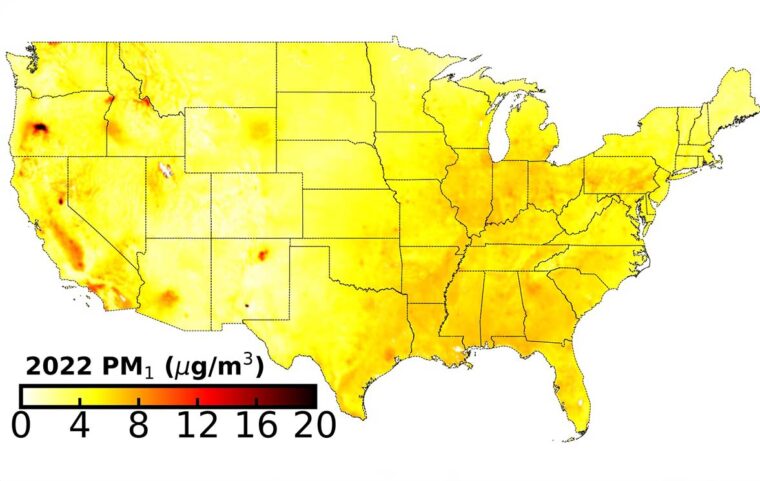
Five hundred ninety wastewater samples were collected from 4 contrasting communities in England between April 2020 and March 2022 to test for antibiotics used, their metabolites, and persistent antibiotic resistance genes (ARGs). Catchment-wide COVID-19 cases and antibiotic prescription data were triangulated with WBE data to evaluate the impact of the COVID-19 pandemic on changes in antibiotic use and resulting AMR at fine spatio-temporal resolution.
Results
Observed reduction in antibiotic consumption and AMR prevalence during the COVID-19 pandemic (especially during lockdowns) is likely due to reduced social interactions rather than due to reduced antibiotic prescribing. Population-normalised daily intake and daily prescriptions showed an increase of 17.2% and 5.8%, respectively, in 2021 to 2022, in comparison to the previous pandemic year. Of the 17 antibiotics targeted, amoxicillin and clarithromycin were clearly affected by COVID-19 restrictions during the years 2020 to 2021 with an average of 31.5% (P < 0.01) and 13.5% (P < 0.05) lower usage, respectively, followed by an increase in 2021 to 2022. This has significant implications for practice and policy that currently focus on the reduction of antibiotics as the key risk factor in AMR.
Conclusions
Better, more holistic strategies encompassing the One Health philosophy are needed to understand and act upon the AMR challenge.